The first Pacemaker was implanted in 1960 and so this technology has now been with us for over half a century.
Multiple developments during that time have made it increasingly sophisticated although they are generally still implanted for the same reasons.
A pacemaker is used to prevent the effects of slow heart rhythms. These often occur with increasing age or due to other cardiac conditions. The different types of slow heart rhythms, or bradycardias, are discussed in the section on Dizzy spells and blackouts as well as how they are diagnosed. Here we will focus on how they are implanted.

More Information:
Pacemaker Implantation
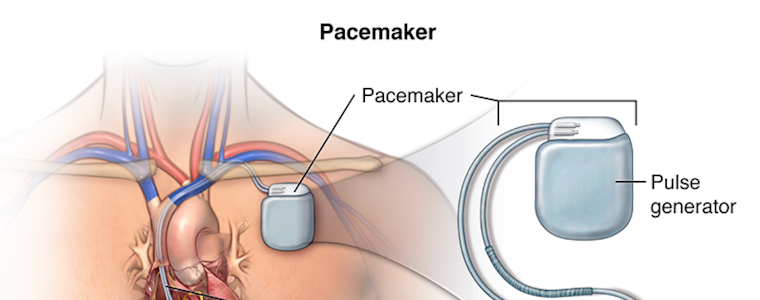
Pacemakers are usually sited under the left collarbone, except in people who are strongly left handed in whom the right side is used. Local anaesthetic is injected into the skin under the left collarbone to make it numb. A small incision is made at this site, usually about 5cm long. The tissues underneath are dissected to create a small pocket under the skin for the pacemaker battery and also to allow identification of a vein suitable to carry the pacemaker leads to the heart.
There are two veins that can be used. One is called the cephalic vein, which is an extension of one of the small veins seen in the crease of the elbow. As it travels up the arm is passes between the shoulder and the chest and can be seen after making the dissection described above. This is generally the best vein to use for inserting pacemaker leads (see below for why) but it is not always possible to use it. This can be because it is too small to use or not straight enough to accept a lead or because it cannot be found. The other vein that is used is called the axillary or subclavian vein. This is a much bigger vein than the cephalic and it carries blood back from the arm to the heart. This vein cannot be seen directly with simple dissection. A needle must be used to gain access to the vein, through which a fine wire can be inserted. The needle is then removed and a plastic sheath is advanced over the wire that allows the pacing lead to be advanced to the heart.
Why is the subclavian vein not as good as the cephalic vein?
There are two main reasons why the cephalic vein is better. Firstly, there is a small risk of injuring the lining of the lung when inserting a needle to find the subclavian vein. This causes the lung to collapse, which is called a pneumothorax. Although not usually dangerous, this often requires insertion of a fine drain into the chest between the ribs to allow the lung to expand. The drain is then removed after 24-48 hours. Rarely surgery may be required. If the needle is advanced to the axillary portion of the subclavian vein, the risk of pneumothorax is very low. The advantage of using the cephalic vein is that there is no risk of causing a pneumothorax because the vein can be seen directly and is not near the lung.
The second reason is that insertion of a pacing lead directly into the subclavian vein can leave it to lie directly between the collarbone and the first rib. If this happens and the spacing between them is very tight, the lead can be constantly rubbed between the two bones causing damage to the lead over time, eventually causing it to fail. This is called subclavian crush. Although the chances of this happening are not very high, this risk is almost zero when using the cephalic vein.
Placing the leads
Once the vein has been accessed, the pacing lead is pushed down the vein into the heart guided by an x-ray camera. Fine metal wires called stylets can be inserted into the lead to help change its shape lead to allow it to be pushed into different positions. The wires can be bent and curled before inserting into the lead to help with this.
Leads are secured by two mechanisms. One is by advancing a small metal screw out of the tip of the lead, called a helix. The helix is designed to screw into the heart tissue itself, thereby anchoring it. Over time scar forms over the tip of the lead holding it in place permanently. This type of lead is called an active fixation lead. The other type of lead, called a passive lead, has simple silicone anchors at the end rather than a helix. I tend not to use this type of lead as it very limited in the number of places the lead can be positioned in the heart. They are also potentially harder to remove in the future if that proves necessary.

The lead is then tested for its ability to record heart signals, called sensing, and its ability to pace the heart, called threshold. If these values are satisfactory, the top of the lead is sewn into the pocket under the collarbone so the lead is then anchored at both ends. If the values are not satisfactory, the helix is retracted and the lead re-positioned.
A second lead may then be added so that both the atrium and the ventricle can be paced although this is not always necessary. For example, patients who have permanent atrial fibrillation (see separate section) cannot have the atrium paced as this rhythm prevents it.
Connecting the Pacemaker
Once the lead, or leads, is in the right position with acceptable values, the other end is inserted into the pacemaker battery, or generator. It is secured by tightening a screw. The pacemaker is then placed in the pocket under the skin and the leads wrapped around it, placing them beneath the generator. I then sew the generator itself to the muscle at the base of the pocket to stop it moving. Many other doctors in the UK choose not to do this, as this is the way it has always been taught here. However, it is customary for this to be done throughout North America and Europe and I believe it prevents a small amount of re-operations to re-position a migrated generator or one that has slipped and causes pain.
Once secured, the pocket and wound are closed with stitches. I use stitches that are slowly absorbed over the next 6 weeks so that you do not need to go back to your doctor to have them removed.
If you are very thin it is often better to place the pacemaker generator under the chest muscle rather than just the skin itself. This protects the generator and prevents it slowly rubbing against the skin as you move about. If this isn’t done it can lead to the generator eroding through the skin, which is a major complication. As cutting through the muscle is painful, I choose to do this with general rather than a local anaesthetic.
Checking the Pacemaker
The pacemaker is then checked once more, this time by placing an antenna directly over the skin, to ensure it is working properly and it is programmed to achieve best results and to use the lowest amount of energy from the pacemaker, so the battery lasts as long as possible. You will then return to the ward and be connected to a heart rhythm monitor. The pacemaker will be checked again later that day or the following day. A chest x-ray will be performed to ensure the leads are in the correct position and there is no lung collapse and if all is satisfactory you will be discharged. The pacemaker is then normally checked again six weeks later.

The pacemaker is then checked at regular intervals, usually once or twice a year. This can be done by attending a pacemaker clinic in London, or potentially closer to home if you live far away.
Another alternative is to have a device at home that can upload information from the pacemaker and transmit it down your phone line. This is called remote monitoring. This is especially useful if you live far away from London or you have difficulty getting to another pacing clinic easily. It also means you can transmit pacemaker data to the clinic if you are concerned by new symptoms or you have reason to worry that your pacemaker is not working properly. Please contact me if you have further questions about remote monitoring.
Complications of pacemaker implantation
Like all operations or procedures, there are several things that can go wrong during or after pacemaker implantation. The accepted overall risk for pacemaker implantation is 1%. In other words, 1 in every 100 people will experience a complication. The following is a list of complications that can occur with pacemaker implantation.
1. Infection
Risk of it happening: 1%
Pacemakers are a foreign body. Bacteria in the air or from other sources can attach themselves to metal or silicone and can cause infection. As antibiotics cannot penetrate metal or silicone, infection can be difficult to treat and it is sometimes necessary to extract the pacemaker and leads. This is a straightforward procedure if the pacemaker leads are less than a year old. Leads that have been in place for many years can be difficult to extract and can require laser or other techniques to perform.
2.Pneumothorax
Risk of it happening: <1%
A pneumothorax is collapse of the lung due to injury to the lining of the lung. This can occur when trying to gain access to the subclavian vein with a needle. The needle can inadvertently injure the lining of the lung causing it to collapse. It can cause breathlessness and is usually easily diagnosed on chest x-ray. The treatment depends on how much the lung collapses. Small collapses can simply be monitored and will heal on their own. Larger collapses require insertion of a fine drain between the ribs to allow the lung to expand. This can usually be removed after a day or two. Rarely it is necessary to perform surgery to repair the hole in the lung lining.
3. Cardiac perforation & tamponade
Risk of it happening: <<1%
This is when the pacemaker lead inadvertently goes through the wall of the heart causing blood to leak out into the sack around the heart, called the pericardium. If small, this can be left. If not small, it requires insertion of a drain into the pericardium using a needle inserted under the ribs. Rarely this can require surgery to correct.
4. Haemothorax
Risk of it happening: <1%
Haemothorax is when bleeding occurs into the chest around the lung. It also occurs on trying to gain access to the subclavian vein with a needle. This complication is rare and is treated by inserting a tube into the lung cavity between the ribs. Surgery may be required to stop the bleeding.
5. Lead displacement
Risk of it happening: 1-2%
A pacemaker lead can move after it has been positioned. Often this means it will not pace properly. This is usually easily detected by the post-operative pacing check or chest x-ray. If the lead has moved and is not pacing properly or appears unstable it will require a repeat procedure to re-position it.
After a pacemaker implant
You should keep your wound covered with a waterproof dressing for a few days. It is important the wound is kept clean and dry to allow it to heal during this time. I almost always use stitches which are dissolvable and gradually dissolve over the next few weeks. If non-dissolvable stitches have been used, they need to be removed after 7 days. You will be informed on discharge whether you need to arrange and appointment for your stitches to be removed
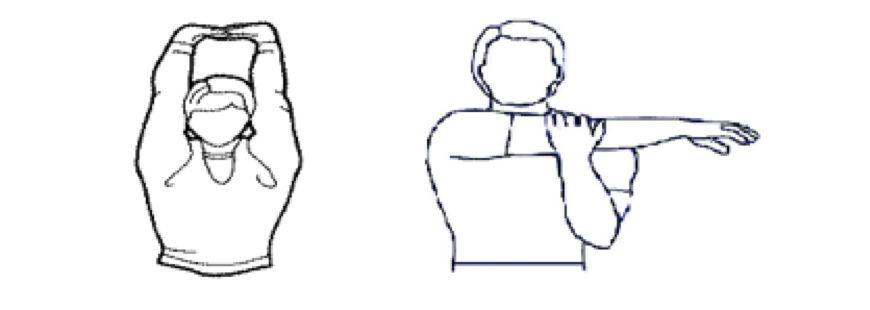
Arm:
You need to be careful with the use of your arm nearest the pacemaker (usually your left arm) for the first 4-6 weeks after your pacemaker implant. This is to prevent the pacemaker leads from moving before they have fully ‘bedded-in’ to the veins & heart. You should avoid lifting your arm above shoulder height on the side your pacemaker is fitted during this time – this is most relevant when putting on T-shirts or jumpers – and not to reach across your body and no heavy lifting (and please see Exercise below).
Driving:
You will be unable to drive for at least a week after pacemaker implantation. You are not required to inform the DVLA of your pacemaker implant for a Group 1 driving license (Cars and Motorcycles). If you hold a Group 2 driving license (Lorries and Buses) you will be unable to drive for 6 weeks. Provided you have no further cardiac conditions, you may be re-licensed after 6 weeks but you DO need to inform the DVLA.
Please note there are different rules for driving if you have an ICD (a defibrillator).
Device follow–up:
The cardiac physiologist and I will program your pacemaker to work the best way for your heart condition. You will see me and a cardiac physiologist again in the pacemaker clinic 4-6 weeks after the implant where we will test pacemaker function, make any programming changes if necessary, ensure your well-being and monitor the battery. After this check, you will need further checks at least once a year for the rest of your life. Sometimes, we need to see you more frequently than this and I will inform you of the reasons for this at the time.
You should inform me:
- If you suspect your pacemaker is no longer functioning correctly. Symptoms may include:
- Fainting
- Severe dizziness/near fainting
- Unexplained falls
- If you have a concern about your device site or wound e.g. it is inflamed, red or discoloured, or if it is starting to come through the skin – call me immediately. It is important to know that GP’s are not experienced in managing pacemakers, which require specialist care.
When should you contact me?
- If you suspect your pacemaker is no longer functioning correctly. Symptoms may include:
- Fainting
- Severe dizziness/near fainting
- Unexplained falls
- If you have a concern about your device site or wound e.g. it is inflamed, red or discoloured, or if it is starting to come through the skin – call me immediately. It is important to know that GP’s are not experienced in managing pacemakers, which require specialist care.
Living with a pacemaker
A pacemaker battery usually lasts between 5-10 years. A variety of factors may affect how long the battery lasts. When you come for a pacemaker check, the battery life on the device will be monitored. As the battery life on your device decreases, the frequency of pacemaker follow-up needs to be increased. This will be discussed with you during your appointment. Before the battery runs out, we will arrange a pacemaker battery replacement procedure.
Exercise
You can gradually return to your normal level of exercise usually very soon after the implant and strenuous exercise after your first pacemaker check 4-6 weeks after implant. You should avoid rough physical contact that could cause you to fall or hit the implant site, as this could potentially damage the device or leads. Contact sport may be problematic. Certain actions which involve big rotations of the left shoulder e.g. swimming, golf, rowing, mountain climbing or specific aerobic exercise involving large arm swings are best avoided, at least for the first 4-6 weeks. This allows the leads to ‘bed in’ properly.
The leads of the pacemaker are the so called ‘weak link’ of the system as they are exposed to repetitive movement both at the shoulder and collar bone and within the beating heart and in some people after many years can lead to fracture. In general, it is best to avoid exposing the lead to high levels of repetitive movement at the shoulder if at all possible to help promote their longevity. This doesn’t mean people should avoid all types of strenuous exercise involving large arm movement, but this should be borne in mind.
Travel
Most people with implanted heart devices can travel freely unless they are restricted by their underlying medical condition. Pacemakers can be checked in >120 countries around the world if problems arise (with contact details available on the manufacturers’ websites).
Airport Security
It is unlikely that screening devices at airports or courts will interfere with your device function or data collection but it is important you let security personnel know you have a pacemaker and show your identification card before walking through an airport security gate. Then, walk through the archway at a normal pace and move away from the system if you feel any dizziness or rapid heartbeats.
Airport security systems are metal detectors, so the alarm may sound when it detects the metal case of your pacemaker. Alternatively, some airport security staff will choose to use an electronic wand to check passengers with pacemakers. Please ask the security attendant to avoid placing or waving the wand back and forth over your device to prevent any malfunction.
Mobile Phone and Other Communication Devices
Wireless communication equipment includes cordless or mobile telephones, pagers, personal digital assistants (PDAs) or other hand-held computers, wi-fi-enabled laptop computers, and bluetooth devices. These may temporarily interact with your pacemaker and affect its function.
Device interaction can be minimised by the following:
- Maintain a distance of at least 6 inches between the equipment and the pacemaker implant site
- When using a mobile phone, hold it to the ear on the opposite side of your implant site
- Don’t carry the phone or other transmitting device in a pocket on the same side as your pacemaker device site or in a shoulder bag near it – some phones emit signals even when they are not in use
Electronic anti-theft systems
Many retail stores and libraries are equipped with electronic surveillance gates to prevent theft. To reduce the chances of these systems affecting your device’s data collection, avoid prolonged exposure while passing through the gates. Simply walk through these systems at a normal pace.
Home Environment
Your pacemaker is not affected by most household electrical equipment such as household appliances, microwave ovens, electrical items for personal care and cleaning, power tools, and home electronics. If you use an induction cook top, you should keep your pacemaker at least 24 inches away from the heating zone when the induction cooktop is on. Conventional heating elements do not affect your insertable cardiac monitor collection data.
Industrial Equipment
Working with or near certain industrial equipment such as arc welding tools, power plants, transmission lines, and other sources of high electrical current can interfere with pacemaker function. Please let me know if you are likely to be exposed to any of these potential sources of strong electromagnetic radiation as this has major implications.
Medical and Dental Procedures
Always tell medical and dental personnel you have a pacemaker. Having a pacemaker device does not prevent you from undergoing medical and dental procedures. With proper precautions, most procedures are unlikely to interfere with its function. However, some medical procedures may temporarily affect the ability of the device to function properly. Some procedures require your doctor or cardiac physiologist to retrieve information from your pacemaker and change the programming prior to and following the procedure. These may include:
- Radiotherapy
- Electrocautery or diathermy (high frequency, short wave or microwave)
- Catheter ablation
- Transcutaneous Electrical Nerve Stimulation (TENS)
- Transurethral needle ablation
- Magnetic resonance imaging (MRI) scans
It is very important to let me know if you are offered treatment with a deep brain or sacral nerve stimulator (neuro-stimulator) as these can potentially interact with a pacemaker and significantly affect its function.
Can I have an MRI or CT scan with a pacemaker?
Almost all currently available, modern pacemakers and leads in the UK have now been tested for compatibility with MRI-scanning if appropriate precautions are taken, depending on pacemaker and MRI type and reason for its use . Patients must usually wait at least 6 weeks after device insertion before an MRI, to allow sufficient time for wound healing. It is very important you let MRI clinic staff know you have a pacemaker device and present your device certification card to them. MRI scans can only be performed safely if such a device is checked and temporarily re-programmed by an appropriately trained cardiac physiologist or cardiologist before and after the MRI scan and cardiac monitoring equipment is available in the MRI unit. It is still common to find many MRI scanning centres will not accept patients wit pacemakers, but some specialise in this area and have built up a great deal of expertise – please contact me before finalising any plans you have to have an MRI.
Older pacemakers and leads have not usually been tested in MRI scanners and the safety of undergoing an MRI scan with an older device cannot always be determined beforehand. It is very important this is only arranged once the appropriate planning and precautions have been arranged, if the scan is thought to be appropriate.
CT scanning is generally safe, although there have been rare reports of CT scans causing pacemaker malfunction and inducing dizzy spells and therefore radiation exposure to the pacemaker area should be minimised.
ICD Implantation
ICDs are implanted in a very similar way to pacemakers. The main differences are the size and characteristics of the leads and the size and shape of the ICD generator. ICD leads are usually slightly thicker than pacing leads. This is because they contain coils to deliver a shock to the heart as well as the components to pace the heart. ICD leads can have one or two shocking coils. The number of coils required is usually dependent on the size and function of your heart. The larger size of the ICD generator means it is more frequently placed below the chest muscle than pacemakers.
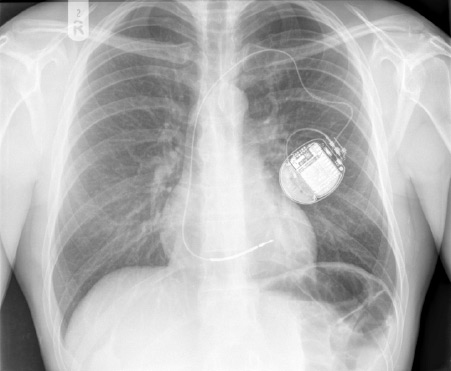
An x-ray showing an active fixation ICD lead attached to a single chamber ICD. The ICD lead has a single shocking coil.
Checking the ICD after implantation
Unlike most current pacemakers, modern ICDs can communicate with an ICD programmer wirelessly if within a few metres of the patient. Although this makes checking the ICD a little bit easier when having a physical ICD check, it really comes into its own with remote monitoring. Patients can choose to have their ICD monitored remotely, again with a device provided which plugs into a telephone line at home. However, unlike a pacemaker, the ICD communicates wirelessly with this device several times a day and will transmit information every night. This means that whenever there is a problem with the ICD or if it has delivered a shock, it will transmit that information to a remote sever. This, in turn, will be notified to me via email by the next working day. This provides greater peace of mind for patients with ICDs and alerts me to problems much more quickly than normal. If you do not wish to have remote monitoring, you will need at least two physical ICD checks each year.
Living with an ICD
In general, the same advice applies for living with an ICD as with pacemakers, as detailed above. One of the key differences with an ICD is that exposure to anything which can potentially cause malfunction could either lead to it delivering a shock (causing pain and more rarely a change in heart rhythm) or preventing it from delivering a shock (leading to failure to treat a life-threatening rhythm, which could potentially lead to death). ICDs have been much less extensively tested in MRI scanners and only a few models are currently ‘MRI-conditional’, although this will rapidly change. It is more difficult to perform MRI scans in patients with ICDs, but it is still possible if the right precautions are taken and need for doing so is justified. It is critical that patients with ICDs contact their cardiologist before undergoing medical procedures or potentially exposing themselves to any of the risks outlined above.
Driving:
You will be unable to drive for at least a month after ICD implantation. You are required to inform the DVLA of your ICD implant in many instances if you are a Group 1 driving license (Cars and Motorcycles) and always if you hold a Group 2 driving license (Lorries and Buses), when you will most likely be re-licensed at this level again. It is very important you do not drive until you have discussed this with me first and are clear whether you need to inform the DVLA or not.
Biventricular pacemakers and ICDs
A biventricular device is one that has leads in both ventricles. This type of device is used to help improve heart function in people with heart failure and who have a specific problem with the heart’s conduction system called left bundle branch block. This causes dyscoordinate contraction of the left ventricle. This is somewhat analogous to a problem with the timing of a car engine. The car will still drive but not very efficiently. By correcting the timing, the function of the heart can improve and in some people it can even go back to normal.
Implanting a left ventricular lead
Implanting a lead in the left ventricle is technically more challenging than in the right ventricle. This is because access to the left ventricle via the veins is only via the veins that feed the back of the heart. These veins need to be accessed with special catheters and special leads are used which are designed to stay inside these veins. This means that procedures to implant a biventricular pacemaker or ICD usually take longer at least an hour longer than a normal pacemaker or ICD. I therefore often choose to perform these procedures with a general anaesthetic. As these leads are more difficult to place and also because they do not have screws (or helixes) securing them, the rate at which they displace is higher than for other types of lead. The rate for other types of complication is very similar to pacemaker implants.